Aetna Medical Prior Authorization Form Explained: Codes, Units, and Site of Care
- Jamie P
- Sep 15, 2025
- 8 min read
When you submit a medical prior authorization (PA) to Aetna—whether for imaging, a procedure, durable medical equipment (DME), or an infusion—the fastest approvals come from clean forms that get three things exactly right: codes, units, and site of care. Miss any of those—or mismatch them against your attachments—and you’ll face pends, denials, or rescheduling headaches.
This guide shows you precisely how to complete Aetna’s medical PA request (via portal or PDF form), what to attach so reviewers can approve on the first submission, and how to calculate units without guesswork. You’ll also get practical checklists, real-world examples, and a one-page template you can drop into your SOP today.
Medical Versus Pharmacy Prior Authorization
Before you fill anything out, confirm which benefit you’re under:
Medical PA covers procedures, imaging, surgeries, DME/orthotics, outpatient facility–administered drugs, and therapy services billed with CPT/HCPCS on a professional (1500) or facility (UB-04) claim. These requests go through Aetna’s provider portal workflow or, when applicable, a downloadable medical authorization form plus attachments.
Pharmacy PA covers retail or specialty prescriptions billed by NDC at a pharmacy. That’s a different process with its own portal/ePA path and forms.
This article focuses on Aetna medical PA submissions—where correct codes, units, and site of care make or break the review.
The Anatomy of a Clean Aetna Medical PA Submission
Think like a reviewer: your job is to validate medical necessity and policy fit quickly. A one-page summary plus labeled attachments is the fastest way to “yes.”
Member and Coverage Snapshot
Member name, DOB, Aetna ID
Product type (commercial, Medicare Advantage, Medicaid), which drives criteria and timelines
Referring and rendering provider names, NPIs, TINs, and contact numbers
Facility name and NPI (if applicable)
Exact Services Requested (Codes and Units)
CPT/HCPCS codes and units for each service
Laterality or modifiers when relevant (e.g., RT/LT, 50, 26/TC)
Planned date(s) of service and place of service (POS)
Diagnosis and Severity
ICD-10 codes aligned to the requested service
Function-forward one-paragraph severity snapshot (e.g., ADL limits, risks, quantified scores when useful)
Conservative Care and Outcomes
Named interventions with dates/durations (e.g., PT 6 weeks, NSAIDs 8 weeks, injections)
Objective outcomes (validated scales, range of motion, frequency/severity logs)
Contraindications or adverse events to alternatives
Evidence Attachments
Reports, not just orders: radiology impressions, sleep study summaries, lab results, specialist consult notes
Relevant baseline tests (e.g., infection screening, organ function reports) tied to risk management
Medical Necessity Rationale and Monitoring
Tie facts to expected policy criteria—no literature dump
Risk plan (peri-procedural, anesthesia, discharge) and objective follow-up milestones
Formatting tip: Use bold micro-headings (Diagnosis, Conservative Care, Imaging/Labs, Rationale, Risk/Follow-Up) in the one-page summary; attach reports separately. Consistency across form, summary, and attachments is non-negotiable.
Codes: How To Choose and Present Them Correctly
CPT/HCPCS for the Service
Primary procedure code(s): the main thing you’re requesting (e.g., 29881 Arthroscopy, knee, meniscectomy).
Add-on codes: list separately and include units (e.g., additional levels in spine procedures).
Device/DME codes: HCPCS (e.g., L-codes) with modifiers when required.
Modifiers and Components Matter
Professional vs. technical: For imaging and diagnostic tests, be clear whether you’re requesting global (no modifier), professional (–26), or technical (–TC) components.
Laterality and multiple procedures: Use RT/LT, 50 for bilateral, or site-specific modifiers when the policy requires explicit laterality.
Policy-driven modifiers: Some services (e.g., therapy) expect GP/GO/GN or other discipline-specific markers; include them where applicable.
Diagnosis Linkage
Pair each CPT/HCPCS with the ICD-10 code that justifies it. Many reviewers (and automated rules) key off medically necessary pairings; mismatches trigger pends.
Explore: Decoding Medical Codes: The Beginner’s Guide to Healthcare Procedure Codes (ICD, CPT, HCPCS)
Units: How To Calculate Them Without Guesswork
Units tell Aetna how much of a service you’re requesting. Errors here are among the top causes of pends.
Time-Based Versus Quantity-Based Codes
Time-based codes (e.g., many therapy and prolonged services) require you to convert total minutes into units using the code descriptor and payer rounding rules. A common clinic standard is the 8-minute rule for certain therapy codes, but always follow the descriptor and plan guidance.
Quantity-based codes (e.g., injections per site, supply items, DME components) reflect number of items or anatomic units rather than minutes.
Imaging and Procedure Units
Modalities like CT/MRI are often 1 unit per complete service. Add-on sequences or bilateral instructions should be coded per descriptor; if the policy expects bilateral with modifier 50, units may remain 1 with the modifier rather than 2—follow your code book and payer rules.
Drug/Dose–Linked HCPCS Units (When Billed on Medical Benefit)
Some facility-administered drugs use HCPCS J-codes with units equal to labeled dosage increments (e.g., “per 10 mg”). Multiply the planned dose by the HCPCS increment to derive units; show your math in the summary to prevent pends.
Document Your Unit Math
A single line saves days:
“Requesting Jxxxx 300 mg; HCPCS unit is 10 mg, therefore 30 units per dose, 1 dose planned on DOS.”
Site of Care: Getting It Right and Documenting Why
Where the service happens is clinically and financially material—and Aetna may have site-of-care policies for safety and cost management.
Common Places of Service (POS)
11 Office (professional setting)
22 Outpatient Hospital (HOPD)
24 Ambulatory Surgery Center (ASC)
12 Home (for home infusions or certain therapies)
31/32 SNF/Nursing Facility (when applicable)
Choosing a Site (and Supporting It)
ASC vs. HOPD: If you select HOPD for a service often done in ASC/office, justify clinical risk factors (airway, comorbidities, anticoagulation, equipment needs).
Home Infusion: Address safety, caregiver capacity, and monitoring; include a fallback plan if conditions change.
Office vs. Facility: For injections/infusions, explain stability, history of reactions, and rescue capability where needed.
Facility Identifiers
Always include the facility NPI and address. If you change facilities after approval, you’ll likely need to update the authorization—don’t assume it auto-transfers.
Related: Prior Authorization Simplified: Reducing Delays in Patient Treatment
Real-World Examples: Codes, Units, and Site of Care
Outpatient Knee Arthroscopy (Meniscectomy)
Codes: 29881 (primary); add 29882 if additional compartment resections are planned
Units: Usually 1 per code; document any add-ons
Site of Care: ASC preferred when appropriate; justify HOPD if comorbidities require hospital resources
Attachments: MRI report showing tear characteristics; PT dates/outcomes; anti-inflammatory/injection history; ortho consult
Summary Tip: “Fails conservative therapy (dates), functional limits (e.g., ambulation <100 ft), MRI confirms [details]; ASC appropriate; anesthesia risk ASA II.”
Facility-Based Sleep Study (PSG) for Adults
Codes: 95810 (diagnostic), 95811 (split-night/titration)
Units: 1
Site of Care: Outpatient hospital sleep lab or accredited center; justify PSG vs. HSAT if applicable
Attachments: ESS score/clinic note; comorbidities (e.g., COPD, neuromuscular disorders) that reduce HSAT accuracy; any prior HSAT report
Summary Tip: “HSAT inconclusive on [date]; PSG indicated due to comorbid COPD and suspected hypoventilation.”
DME: Custom Knee Orthosis
Code: L1846 (example; confirm exact device)
Units: Typically 1
Site of Care: Fitted in office; device billed under medical benefit
Attachments: Ortho evaluation (measurements, gait analysis), off-the-shelf brace failure with dates and outcomes
Summary Tip: “Objective improvement predicted in ambulation safety; caregiver education plan included.”
Infused Therapy Under Medical Benefit
Codes: J-codes for the drug (dose-based units) + CPT administration code(s)
Units: Derive from mg per HCPCS unit; show math
Site of Care: Office, infusion center, or home infusion (if permitted); justify rescue/anaphylaxis readiness
Attachments: Baseline labs, infection screens, prior therapies with outcomes/contraindications
Summary Tip: “Prior agents tried/failed (dates); baseline TB negative; dosing 300 mg → 30 units of Jxxxx per dose; office infusion with rescue meds and monitoring.”
What To Attach: Reports, Not Orders
Attach reports that show results (radiology impressions, lab values, consult assessments), not just orders or scheduling notes. For therapy/DME, attach treatment logs, measurements, and objective outcomes (e.g., validated scales or timed tests). Label files clearly (e.g., “MRI_RightKnee_2025-02-12.pdf”).
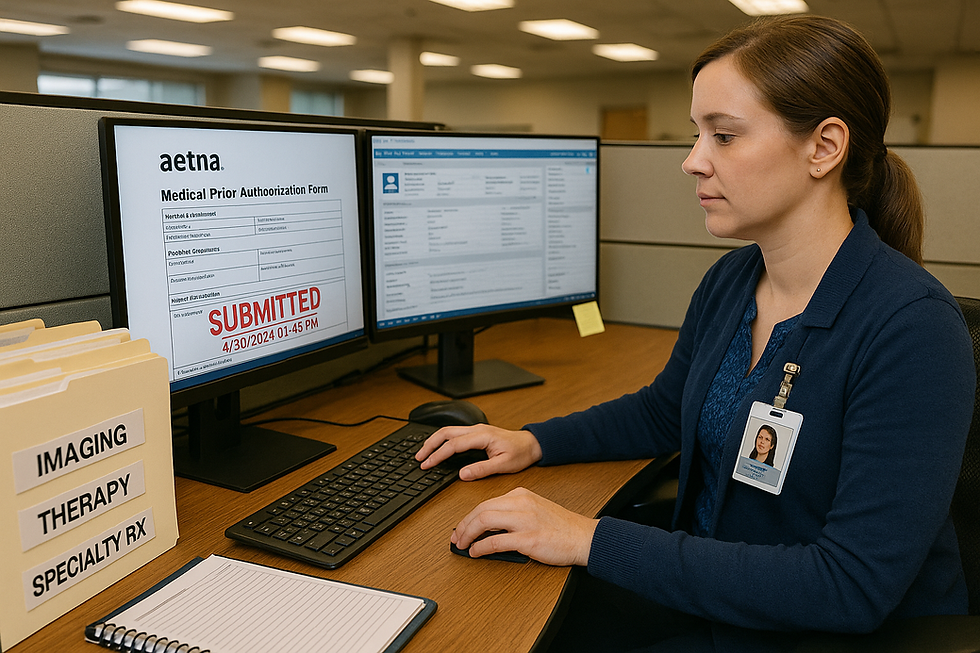
Completing Aetna’s Medical PA: Portal Versus Form
Portal (Preferred)
Structured fields reduce missing data.
You’ll get a confirmation number and posted turnaround window.
Upload your one-page summary and attachments directly.
PDF Form (When Required)
Download the current form for the service line/product.
Complete all fields (member, provider, codes/units, POS, DOS).
Attach your summary and evidence.
Submit through the designated channel (fax/portal upload) indicated on the form or site.
Consistency is king: Codes, units, site of care, and dates must match across the form, one-pager, attachments, and orders.
Timelines and Follow-Ups
Turnaround depends on product and service type. Keep momentum:
Submit a complete packet on day one.
Save the confirmation ID and posted timeframe.
Set a follow-up two business days before the window closes.
If pended, upload exactly what’s requested the same day with a two-line note referencing the case number and attachment names.
If denied, decide quickly: peer-to-peer (for clinical nuance) or internal appeal with a point-by-point cover letter.
The “No-Pend” Checklist
Member/Plan info complete; product type confirmed
Referring/Rendering/Facility names, NPIs, TINs correct
CPT/HCPCS codes and units accurate; modifiers applied where needed
ICD-10 codes align to services
Place of Service and facility NPI listed; site-of-care rationale included if sensitive
Dates of Service consistent across form, summary, and orders
Reports Attached: Imaging/labs/consults (not just orders)
Conservative Care named with dates/durations/outcomes
One-Page Summary with headings and tie-back to policy criteria
Direct Callback for reviewer questions provided
Template: One-Page Medical Necessity Summary
Patient / Plan: [Name, DOB, Aetna ID, product type]
Service: [CPT/HCPCS + units, POS/facility NPI, DOS]
Diagnosis & Severity: [ICD-10] + brief function-forward snapshot (ADL limits, quantified scores, risks)
Conservative Treatment: [Named interventions + dates/durations; outcomes; adverse events/contraindications]
Imaging/Labs/Consults: [Report names + dates + key findings]
Rationale: [Point-by-point tie to policy criteria; why now; expected benefit]
Risk & Follow-Up: [Peri-procedural/anesthesia plan, discharge, objective follow-up timeline]
Unit Math (if any): [e.g., Jxxxx per 10 mg; dose 300 mg → 30 units]
Avoid These High-Friction Mistakes
Dose/Unit Mismatches: J-code math that doesn’t equal the ordered dose; fix with a one-line calculation.
Orders Instead of Reports: Upload imaging reports, not orders; same for sleep studies and labs.
Vague Conservative Care: “Failed PT” isn’t enough—include dates, sessions, and measured results.
Unjustified Site of Care: HOPD selected for a procedure typically done in ASC without clinical rationale; add risk/context.
Wrong Channel: Some services route through specific programs/vendors; use the channel the plan specifies.
Unreachable Clinical Contact: Provide a direct line for reviewer callbacks; missed calls cost days.
Building a Small “PA Pod” for Reliability
You don’t need a large team—just clear ownership and repeatable checklists:
Intake & Routing: Verifies benefit/product, confirms PA requirement per code, selects channel, captures facility details.
Clinical Packager: Drafts the one-page summary; compiles reports/logs; checks consistency for codes/units/POS.
Tracker & Escalations: Logs confirmation IDs, monitors deadlines, triggers follow-ups, schedules peer-to-peers or appeals.
Hold a 15-minute weekly huddle to review “Pending > 3 Business Days” and knock out the top three causes of delay.
Frequently Asked Questions
Do all Aetna plans use the same PA rules?
No. Requirements vary by product (commercial, Medicare Advantage, Medicaid) and state. Always check by plan and by code before scheduling.
Do approvals expire?
Yes—most authorizations are time-bound or unit-bound. Rescheduling beyond the window or increasing units usually requires an update or extension.
What if I change the facility?
Update the authorization with the new facility NPI/POS. Don’t assume transferability.
When should I request expedited review?
When delay risks serious harm or functional loss. State the concrete clinical reason and reference the supporting reports.
Is a peer-to-peer available?
Often yes. Use it when medical necessity turns on clinical nuance (safety, atypical presentation, failed alternatives).
About OpsArmy
OpsArmy builds AI-native, fully managed back-office teams so companies can run day-to-day operations with precision—from sales development and admin to finance and hiring.
Learn more at https://operationsarmy.com



Comments